PRP可用於協助處理放射治療所引起的放射性傷口
PRP可用於協助處理放射治療所引起的放射性傷口
實驗證實PRP有助於放射治療所引起的皮膚傷口癒合之細胞修復,因PRP 製劑內含有血小板衍生生長因子 (PDGF-AB)、血管內皮生長因子 (VEGF)、bFGF 和高濃度的 sICAM-1。
PRP科技新知- PRP可用於協助處理放射治療所引起的放射性傷口
研究背景:
放射治療傷口癒合不佳的主要原因是微血管損傷,由於富含血小板血漿 (PRP)具有促進血管新生成功能,因此目前建議將PRP產品用於治療慢性傷口。
研究目的: PRP 對於放射治療所引起的皮膚傷口癒合過程的細胞修復影響。
材料與方法:
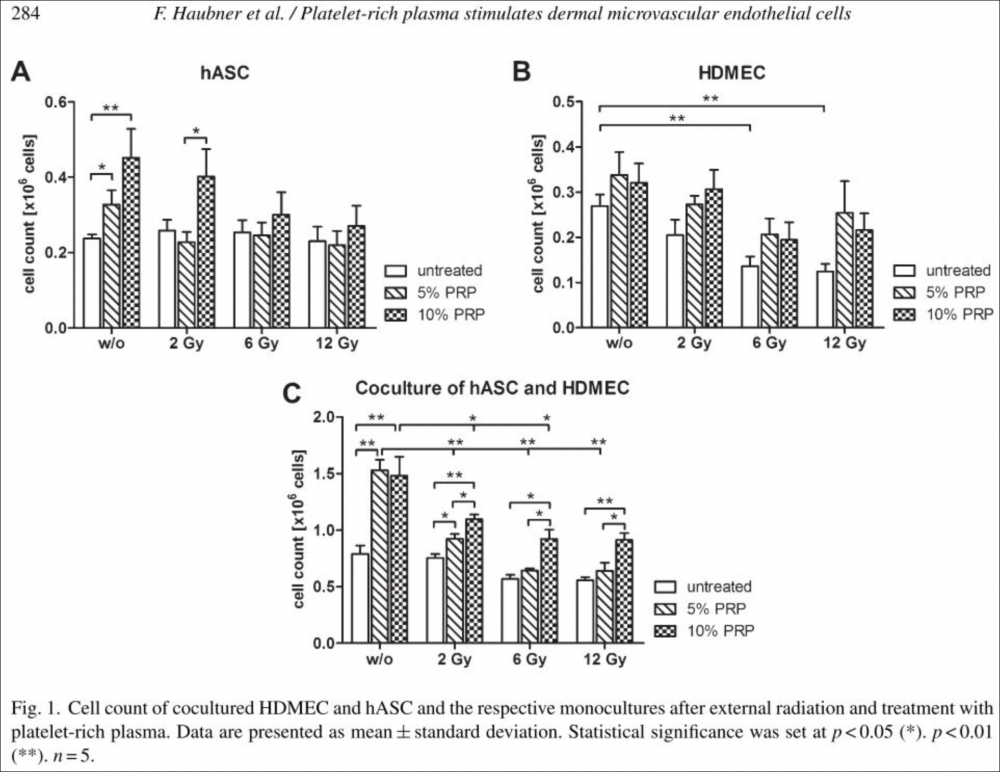
培養人類真皮微血管內皮細胞(HDMEC)和人類脂肪幹細胞(hASC),並使用2至12 格雷 (Gy) 的放射治療劑量。在放射治療上述細胞後,加入不同濃度PRP,並在放射治療照射後 48 小時使用半自動細胞計數器來計算細胞總數。通過酶聯免疫吸附試驗(ELISA)測定 HDMEC 和 hASC 培養物上清液中的白細胞介素 6 (IL-6)、纖維母細胞生長因子(bFGF)和可溶性細胞間粘附分子 1 (sICAM-1)。沒有接受輻射線的 hASC 和 HDMEC 作為對照組。
結果:
PRP 製劑內含有血小板衍生生長因子 (PDGF-AB)、血管內皮生長因子 (VEGF)、bFGF 和高濃度的 sICAM-1。將 PRP 添加到經過放射治療照射後的 HDMEC 和 hASC 的培養物中可防止放射治療所引起的細胞數量的嚴重下降。 使用10% PRP 可將細胞數量恢復到未放射治療前的細胞數目。將10% PRP 加入沒有放射治療、和用 6 Gy、12 Gy 照射後處理的 hASC 單一培養物中, bFGF 表達顯著降低。在 HDMEC 中也觀察到 PRP 的這些抑制作用。相比之下,HDMEC-ASC 的共同培養物在用 5% 或 10% PRP 處理時顯示出 bFGF 表達的劑量依賴性增加。 6 Gy 和 12 Gy 的放射治療劑量增加了用 5% PRP 刺激的培養物中的 IL-6 表達。
結論:在 hASC 和 HDMEC 的共同培養中加入 PRP,可誘導 bFGF 並恢復因放射治療所引起的增殖缺陷。在放射治療條件下,PRP 可能會誘導促炎刺激,這可能有利於治療癒合過程有缺陷的慢性傷口。 hASC 和 PRP 產品的聯合使用可能有助於治療放射性傷口。
原文摘要:
BACKGROUND: Platelet-rich plasma (PRP) products are currently suggested in the treatment of chronic wounds due to possible pro-angiogenic effects. Microvascular compromise represents the major component in radiogenic wound healing complications. The effects of PRP on irradiated cells of the cutaneous wound healing process are still poorly understood.
MATERIAL AND METHODS: Human dermal microvascular endothelial cells (HDMEC) and human adipose derived stem cells (hASC) were cultured and irradiated with doses of 2 to 12 Gy. PRP was activated, characterized and added to the incubation media in different concentrations after external radiation. Cell count was determined 48 h after radiation using a semi-automated cell counting system. Levels of interleukin-6 (IL-6), basic fibroblast growth factor (bFGF) and soluble intercellular adhesion molecule-1 (sICAM-1) in the supernatants of HDMEC and hASC co-cultures were determined by enzyme-linked immunosorbent assay (ELISA). Non-irradiated hASC and HDMEC served as controls.
RESULTS: The employed PRP preparations were characterized and contained platelet derived growth factor (PDGF-AB), vascular endothelial growth factor (VEGF), bFGF and high levels of sICAM-1. Addition of PRP to irradiated cultures of HDMEC and hASC prevented profound radiation-induced decline in cell numbers. 10% PRP restored cell numbers to levels of untreated, non-irradiated cultures. Basic FGF expression was decreased significantly in hASC monocultures treated with 10% PRP without external radiation and after irradiation with 6 and 12 Gy. These inhibitory effects of PRP were also observed in HDMEC. In contrast, co-cultures of HDMEC-ASC showed a dose-dependent increase in bFGF expression when treated with 5 or 10% PRP. Doses of 6 and 12 Gy increased IL-6 expression in cultures stimulated with 5% PRP.
CONCLUSIONS: Use of PRP in co-cultures of hASC and HDMEC restores proliferative defects caused by external radiation probably by induction of bFGF. Under irradiated conditions, PRP might induce pro-inflammatory stimuli which could be beneficial in treatment of chronic wounds where healing processes are defective. Combined use of hASC and PRP products might be helpful in the treatment of radiogenic wounds.
文章出處: Haubner F, Muschter D, Schuster N, Pohl F, Ahrens N, Prantl L, Gassner HG: Platelet-rich plasma stimulates dermal microvascular endothelial cells and adipose derived stem cells after external radiation. Clin Hemorheol Microcirc 2015, 61(2):279-290.
研究背景:
放射治療傷口癒合不佳的主要原因是微血管損傷,由於富含血小板血漿 (PRP)具有促進血管新生成功能,因此目前建議將PRP產品用於治療慢性傷口。
研究目的: PRP 對於放射治療所引起的皮膚傷口癒合過程的細胞修復影響。
材料與方法:
培養人類真皮微血管內皮細胞(HDMEC)和人類脂肪幹細胞(hASC),並使用2至12 格雷 (Gy) 的放射治療劑量。在放射治療上述細胞後,加入不同濃度PRP,並在放射治療照射後 48 小時使用半自動細胞計數器來計算細胞總數。通過酶聯免疫吸附試驗(ELISA)測定 HDMEC 和 hASC 培養物上清液中的白細胞介素 6 (IL-6)、纖維母細胞生長因子(bFGF)和可溶性細胞間粘附分子 1 (sICAM-1)。沒有接受輻射線的 hASC 和 HDMEC 作為對照組。
結果:
PRP 製劑內含有血小板衍生生長因子 (PDGF-AB)、血管內皮生長因子 (VEGF)、bFGF 和高濃度的 sICAM-1。將 PRP 添加到經過放射治療照射後的 HDMEC 和 hASC 的培養物中可防止放射治療所引起的細胞數量的嚴重下降。 使用10% PRP 可將細胞數量恢復到未放射治療前的細胞數目。將10% PRP 加入沒有放射治療、和用 6 Gy、12 Gy 照射後處理的 hASC 單一培養物中, bFGF 表達顯著降低。在 HDMEC 中也觀察到 PRP 的這些抑制作用。相比之下,HDMEC-ASC 的共同培養物在用 5% 或 10% PRP 處理時顯示出 bFGF 表達的劑量依賴性增加。 6 Gy 和 12 Gy 的放射治療劑量增加了用 5% PRP 刺激的培養物中的 IL-6 表達。
結論:在 hASC 和 HDMEC 的共同培養中加入 PRP,可誘導 bFGF 並恢復因放射治療所引起的增殖缺陷。在放射治療條件下,PRP 可能會誘導促炎刺激,這可能有利於治療癒合過程有缺陷的慢性傷口。 hASC 和 PRP 產品的聯合使用可能有助於治療放射性傷口。
原文摘要:
BACKGROUND: Platelet-rich plasma (PRP) products are currently suggested in the treatment of chronic wounds due to possible pro-angiogenic effects. Microvascular compromise represents the major component in radiogenic wound healing complications. The effects of PRP on irradiated cells of the cutaneous wound healing process are still poorly understood.
MATERIAL AND METHODS: Human dermal microvascular endothelial cells (HDMEC) and human adipose derived stem cells (hASC) were cultured and irradiated with doses of 2 to 12 Gy. PRP was activated, characterized and added to the incubation media in different concentrations after external radiation. Cell count was determined 48 h after radiation using a semi-automated cell counting system. Levels of interleukin-6 (IL-6), basic fibroblast growth factor (bFGF) and soluble intercellular adhesion molecule-1 (sICAM-1) in the supernatants of HDMEC and hASC co-cultures were determined by enzyme-linked immunosorbent assay (ELISA). Non-irradiated hASC and HDMEC served as controls.
RESULTS: The employed PRP preparations were characterized and contained platelet derived growth factor (PDGF-AB), vascular endothelial growth factor (VEGF), bFGF and high levels of sICAM-1. Addition of PRP to irradiated cultures of HDMEC and hASC prevented profound radiation-induced decline in cell numbers. 10% PRP restored cell numbers to levels of untreated, non-irradiated cultures. Basic FGF expression was decreased significantly in hASC monocultures treated with 10% PRP without external radiation and after irradiation with 6 and 12 Gy. These inhibitory effects of PRP were also observed in HDMEC. In contrast, co-cultures of HDMEC-ASC showed a dose-dependent increase in bFGF expression when treated with 5 or 10% PRP. Doses of 6 and 12 Gy increased IL-6 expression in cultures stimulated with 5% PRP.
CONCLUSIONS: Use of PRP in co-cultures of hASC and HDMEC restores proliferative defects caused by external radiation probably by induction of bFGF. Under irradiated conditions, PRP might induce pro-inflammatory stimuli which could be beneficial in treatment of chronic wounds where healing processes are defective. Combined use of hASC and PRP products might be helpful in the treatment of radiogenic wounds.
文章出處: Haubner F, Muschter D, Schuster N, Pohl F, Ahrens N, Prantl L, Gassner HG: Platelet-rich plasma stimulates dermal microvascular endothelial cells and adipose derived stem cells after external radiation. Clin Hemorheol Microcirc 2015, 61(2):279-290.

