PRP可減輕急性放射治療副作用
PRP可減輕急性放射治療副作用
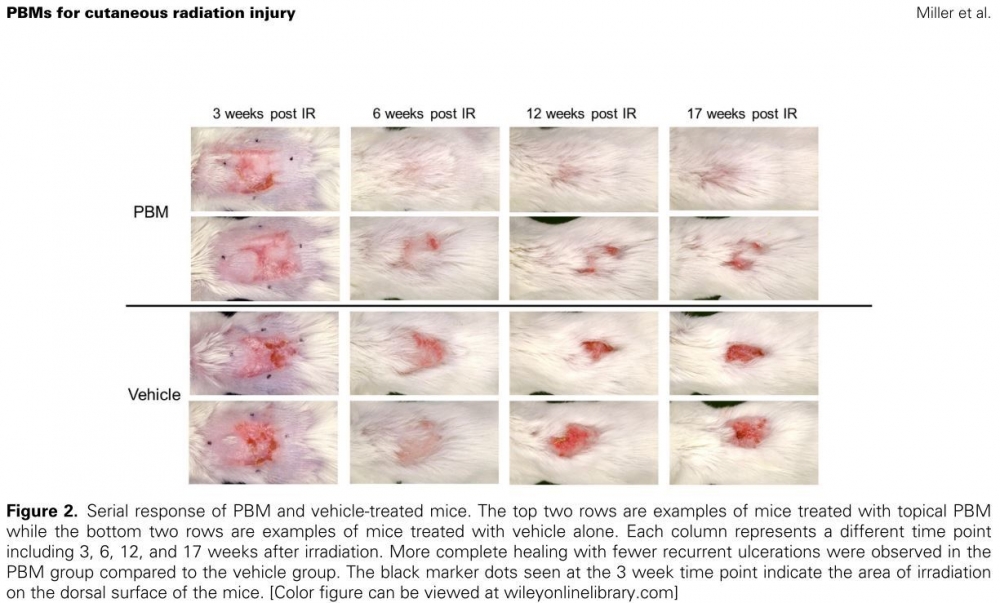
暴露於高劑量放射治療所引起的皮膚傷口是臨床治療的重大挑戰,在這項研究中,使用小鼠模型來研究PRP減少放射性皮膚損傷的急性和晚期副作用,在放射治療後共使用5週。每週成像顯示,使用PRP的傷口恢復更好,得知PRP可有效促進傷口修復,進而減輕急性放射治療副作用。
PRP科技新知- PRP可減輕急性放射治療副作用
研究背景:
暴露於高劑量放射治療所引起的皮膚傷口是臨床治療的重大挑戰。雖然目前有許多新的皮膚治療方式正在研究中,但尚未證實任何皮膚療法可用於治療放射性皮膚炎的損傷或是可以促進受損組織的修復。PRP是由富含血小板的血漿製成的具有生物活性的生物材料 (這篇文章寫做Plasma-based biomaterials, PBMs),可以製成固體和半固體形式,價格相對低廉,可作為現成的非冷藏產品。
研究方法:
在這項研究中,使用小鼠模型來研究PRP減少放射性皮膚損傷的急性和晚期副作用。使用單劑量35格雷(Gy)照射直徑為2公分的背部皮膚照野,然後每天一次使用PRP進行局部治療,在放射治療後共使用5週。每週成像顯示,使用PRP的傷口恢復更好: 在最大傷口面積後第 12、13 和 14 週時變得具有統計學意義 (p < 0.05)。
結論:
PRP可有效促進傷口修復,進而減輕急性放射治療副作用。
原文摘要:
Cutaneous wounds caused by an exposure to high doses of ionizing radiation remain a therapeutic challenge. While new experimental strategies for treatment are being developed, there are currently no off-the-shelf therapies for the treatment of cutaneous radiation injury that have been proven to promote repair of the damaged tissues. Plasma-based biomaterials are biologically active biomaterials made from platelet enriched plasma, which can be made into both solid and semi-solid forms, are inexpensive, and are available as off-the-shelf, non-refrigerated products. In this study, the use of plasma-based biomaterials for the mitigation of acute and late toxicity for cutaneous radiation injury was investigated using a mouse model. A 2-cm diameter circle of the dorsal skin was irradiated with a single dose of 35 Gy followed by topical treatment with plasma-based biomaterial or vehicle once daily for 5 weeks post-irradiation. Weekly imaging demonstrated more complete wound resolution in the plasma-based biomaterial vs. vehicle group which became statistically significant (p < 0.05) at weeks 12, 13, and 14 post-maximum wound area. Despite more complete wound healing, at 9 and 17 weeks post-irradiation, there was no statistically significant difference in collagen deposition or skin thickness between the plasma-based biomaterial and vehicle groups based on Masson trichrome staining nor was there a statistically significant difference in inflammatory or fibrosis-related gene expression between the groups. Although significant improvement was not observed for late toxicity, plasma-based biomaterials were effective at promoting wound closure, thus helping to mitigate acute toxicity.
文章出處:
Miller ED, Song F, Smith JD, Ayan AS, Mo X, Weldon M, Lu L, Campbell PG, Bhatt AD, Chakravarti A et al: Plasma-based biomaterials for the treatment of cutaneous radiation injury. Wound Repair Regen 2019, 27(2):139-149.
研究背景:
暴露於高劑量放射治療所引起的皮膚傷口是臨床治療的重大挑戰。雖然目前有許多新的皮膚治療方式正在研究中,但尚未證實任何皮膚療法可用於治療放射性皮膚炎的損傷或是可以促進受損組織的修復。PRP是由富含血小板的血漿製成的具有生物活性的生物材料 (這篇文章寫做Plasma-based biomaterials, PBMs),可以製成固體和半固體形式,價格相對低廉,可作為現成的非冷藏產品。
研究方法:
在這項研究中,使用小鼠模型來研究PRP減少放射性皮膚損傷的急性和晚期副作用。使用單劑量35格雷(Gy)照射直徑為2公分的背部皮膚照野,然後每天一次使用PRP進行局部治療,在放射治療後共使用5週。每週成像顯示,使用PRP的傷口恢復更好: 在最大傷口面積後第 12、13 和 14 週時變得具有統計學意義 (p < 0.05)。
結論:
PRP可有效促進傷口修復,進而減輕急性放射治療副作用。
原文摘要:
Cutaneous wounds caused by an exposure to high doses of ionizing radiation remain a therapeutic challenge. While new experimental strategies for treatment are being developed, there are currently no off-the-shelf therapies for the treatment of cutaneous radiation injury that have been proven to promote repair of the damaged tissues. Plasma-based biomaterials are biologically active biomaterials made from platelet enriched plasma, which can be made into both solid and semi-solid forms, are inexpensive, and are available as off-the-shelf, non-refrigerated products. In this study, the use of plasma-based biomaterials for the mitigation of acute and late toxicity for cutaneous radiation injury was investigated using a mouse model. A 2-cm diameter circle of the dorsal skin was irradiated with a single dose of 35 Gy followed by topical treatment with plasma-based biomaterial or vehicle once daily for 5 weeks post-irradiation. Weekly imaging demonstrated more complete wound resolution in the plasma-based biomaterial vs. vehicle group which became statistically significant (p < 0.05) at weeks 12, 13, and 14 post-maximum wound area. Despite more complete wound healing, at 9 and 17 weeks post-irradiation, there was no statistically significant difference in collagen deposition or skin thickness between the plasma-based biomaterial and vehicle groups based on Masson trichrome staining nor was there a statistically significant difference in inflammatory or fibrosis-related gene expression between the groups. Although significant improvement was not observed for late toxicity, plasma-based biomaterials were effective at promoting wound closure, thus helping to mitigate acute toxicity.
文章出處:
Miller ED, Song F, Smith JD, Ayan AS, Mo X, Weldon M, Lu L, Campbell PG, Bhatt AD, Chakravarti A et al: Plasma-based biomaterials for the treatment of cutaneous radiation injury. Wound Repair Regen 2019, 27(2):139-149.

