
PRP凝膠可用於放射性皮膚炎的治療
PRP凝膠可用於放射性皮膚炎的治療
放射治療是治療癌症的重要方式,但儘管放射治療技術的進步,仍有 5-15% 患者的健康組織會因暴露於輻射下受到損害,經實驗評估PRP凝膠在慢性放射性皮膚炎的療效證實PRP凝膠對放射性皮膚炎有預防效果。
PRP科技新知 - PRP凝膠可用於放射性皮膚炎的治療
研究背景:
放射治療是治療癌症的重要方式,但儘管放射治療技術的進步,仍有 5-15% 患者的健康組織會因暴露於輻射下受到損害。皮膚和黏膜病變是放射治療的嚴重副作用,對患者的生活品質產生巨大影響。雖然常規外用藥物在急性放射性皮膚炎有效果,但在慢性放射性皮膚副作用仍無法克服。大量基礎和臨床研究發現,局部外用的PRP凝膠能夠藉由血小板α顆粒中所含的各種生長因子的作用來加速組織的再生和修復。因此,此篇文章評估PRP凝膠在慢性放射性皮膚炎的療效。
研究方法:
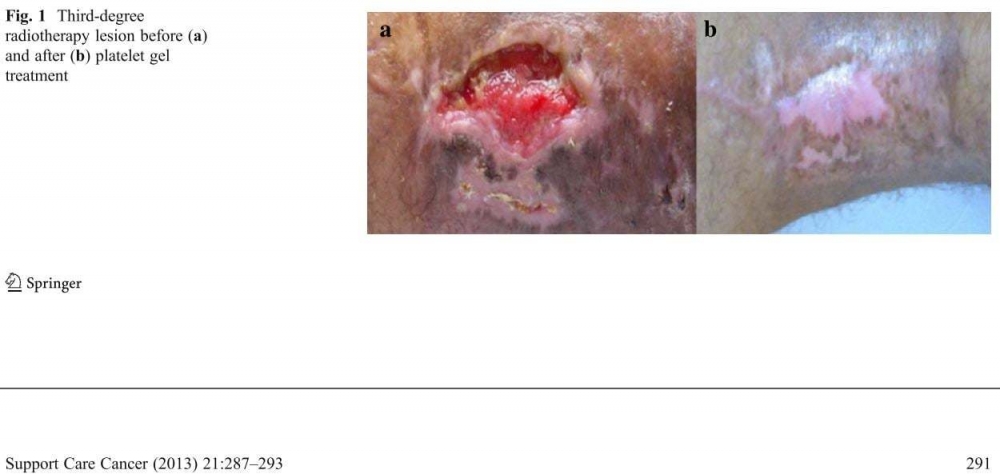
使用凝血酶處理自體抽血所獲得的血小板製備PRP凝膠 [此篇文章的PRP凝膠是利用“自我抽血”的方式製備而成]。通過微生物測試確保產品的安全性。自體血小板凝膠每週一次局部使用,平均持續時間為 35 天,用於治療慢性三度和四度放射性皮膚炎 (歐洲壓瘡諮詢小組分類EPUAP和不良事件通用術語標準評分CTCAE)。 10 名患者先前通過腫瘤切除和術後放射治療(劑量 50-64 格雷)中度至高度(Grade 2-3)肢體惡性肉瘤。
結果:
放射性皮膚炎在治療後的不同時期出現,並且都證明PRP凝膠對放射性皮膚炎有預防效果。在接受放射治療的 10 名患者中有 7 名發現PRP凝膠可以成功預防和治療放射性皮膚炎。PRP凝膠在所有病人的各個階段都有癒合效果。在 5 年的追蹤過程,7 名成功治療的患者中有 6 名既沒有疾病也沒有皮膚病變。
結論:PRP凝膠可用於慢性放射性皮膚炎的治療,並可減少所需的皮膚藥物與住院次數,進而有助於提高患者的依從性和有利的成本/效益比。
原文摘要:
INTRODUCTION: Radiotherapy, alone or in combination with chemotherapy and/or surgery, is a fundamental and irreplaceable method of treating tumours. Nonetheless, although the technological advances made during recent years and the associated improvements in this type of treatment have reduced the incidence of complications, 5-15 % of patients still experience damage to the healthy tissues exposed to radiation. Cutaneous and mucosal lesions are severe collateral effects of radiotherapy that have an enormous impact on a patient's quality of life. Unfortunately, however, the efficacy of conventional treatments, while demonstrably useful in acute lesions, remains disputed in chronic cases. Nevertheless, numerous studies and clinical findings have demonstrated that topical, non-transfusional plasma-rich platelet gel is able to accelerate the regeneration and repair of tissues through the action of the various growth factors contained within the alpha granules of platelets. We therefore set out to evaluate the efficacy of autologous platelet gel, chosen for its limited cost and ease of preparation, in chronic cutaneous radiation dermatitis.
METHODS: "Home-made" platelet gel was produced by treating platelets with autologous thrombin. The safety of the product was ensured by microbiological tests. The autologous platelet gel was applied topically once a week, for a mean duration of 35 days, to chronic third- and fourth-degree (European Pressure Ulcer Advisory Panel classification and Common Terminology Criteria for Adverse Events score) cutaneous radiation dermatitis in a group of ten patients previously treated for moderate-to-high grade (histology G2-G3) limb sarcoma by tumour excision and post-surgical radiotherapy (dose 50-64 Gy). The radiation dermatitis had appeared at different intervals after treatment and had all proved resistant to conventional treatments.
RESULTS: The autologous platelet gel was found to be successful in seven out of the ten patients treated. The various phases of the healing process were observed in all cases. Platelet gel application was suspended in three patients: in one patient after one application due to tumour progression, in another patient after two applications due to development of distant metastases and in the third after six applications with only partial tissue response. At 5-year follow-up, six of the seven successfully treated patients remained free of both disease and lesion, while the remaining patient, the eldest, had passed away in the interim due to extraneous causes.
CONCLUSION: Platelet gel treatment could therefore be used to bring about healing in chronic cutaneous radiation dermatitis, lending itself to better patient compliance and a favourable cost/benefit ratio, due to a reduction in the number of medications and hospital visits required.
文章出處: Lervolino V, Di Costanzo G, Azzaro R, Diodato AM, Di Macchia CA, Di Meo T, Petruzziello A, Loquercio G, Muto P, Apice G et al: Platelet gel in cutaneous radiation dermatitis. Support Care Cancer 2013, 21(1):287-293.
研究背景:
放射治療是治療癌症的重要方式,但儘管放射治療技術的進步,仍有 5-15% 患者的健康組織會因暴露於輻射下受到損害。皮膚和黏膜病變是放射治療的嚴重副作用,對患者的生活品質產生巨大影響。雖然常規外用藥物在急性放射性皮膚炎有效果,但在慢性放射性皮膚副作用仍無法克服。大量基礎和臨床研究發現,局部外用的PRP凝膠能夠藉由血小板α顆粒中所含的各種生長因子的作用來加速組織的再生和修復。因此,此篇文章評估PRP凝膠在慢性放射性皮膚炎的療效。
研究方法:
使用凝血酶處理自體抽血所獲得的血小板製備PRP凝膠 [此篇文章的PRP凝膠是利用“自我抽血”的方式製備而成]。通過微生物測試確保產品的安全性。自體血小板凝膠每週一次局部使用,平均持續時間為 35 天,用於治療慢性三度和四度放射性皮膚炎 (歐洲壓瘡諮詢小組分類EPUAP和不良事件通用術語標準評分CTCAE)。 10 名患者先前通過腫瘤切除和術後放射治療(劑量 50-64 格雷)中度至高度(Grade 2-3)肢體惡性肉瘤。
結果:
放射性皮膚炎在治療後的不同時期出現,並且都證明PRP凝膠對放射性皮膚炎有預防效果。在接受放射治療的 10 名患者中有 7 名發現PRP凝膠可以成功預防和治療放射性皮膚炎。PRP凝膠在所有病人的各個階段都有癒合效果。在 5 年的追蹤過程,7 名成功治療的患者中有 6 名既沒有疾病也沒有皮膚病變。
結論:PRP凝膠可用於慢性放射性皮膚炎的治療,並可減少所需的皮膚藥物與住院次數,進而有助於提高患者的依從性和有利的成本/效益比。
原文摘要:
INTRODUCTION: Radiotherapy, alone or in combination with chemotherapy and/or surgery, is a fundamental and irreplaceable method of treating tumours. Nonetheless, although the technological advances made during recent years and the associated improvements in this type of treatment have reduced the incidence of complications, 5-15 % of patients still experience damage to the healthy tissues exposed to radiation. Cutaneous and mucosal lesions are severe collateral effects of radiotherapy that have an enormous impact on a patient's quality of life. Unfortunately, however, the efficacy of conventional treatments, while demonstrably useful in acute lesions, remains disputed in chronic cases. Nevertheless, numerous studies and clinical findings have demonstrated that topical, non-transfusional plasma-rich platelet gel is able to accelerate the regeneration and repair of tissues through the action of the various growth factors contained within the alpha granules of platelets. We therefore set out to evaluate the efficacy of autologous platelet gel, chosen for its limited cost and ease of preparation, in chronic cutaneous radiation dermatitis.
METHODS: "Home-made" platelet gel was produced by treating platelets with autologous thrombin. The safety of the product was ensured by microbiological tests. The autologous platelet gel was applied topically once a week, for a mean duration of 35 days, to chronic third- and fourth-degree (European Pressure Ulcer Advisory Panel classification and Common Terminology Criteria for Adverse Events score) cutaneous radiation dermatitis in a group of ten patients previously treated for moderate-to-high grade (histology G2-G3) limb sarcoma by tumour excision and post-surgical radiotherapy (dose 50-64 Gy). The radiation dermatitis had appeared at different intervals after treatment and had all proved resistant to conventional treatments.
RESULTS: The autologous platelet gel was found to be successful in seven out of the ten patients treated. The various phases of the healing process were observed in all cases. Platelet gel application was suspended in three patients: in one patient after one application due to tumour progression, in another patient after two applications due to development of distant metastases and in the third after six applications with only partial tissue response. At 5-year follow-up, six of the seven successfully treated patients remained free of both disease and lesion, while the remaining patient, the eldest, had passed away in the interim due to extraneous causes.
CONCLUSION: Platelet gel treatment could therefore be used to bring about healing in chronic cutaneous radiation dermatitis, lending itself to better patient compliance and a favourable cost/benefit ratio, due to a reduction in the number of medications and hospital visits required.
文章出處: Lervolino V, Di Costanzo G, Azzaro R, Diodato AM, Di Macchia CA, Di Meo T, Petruzziello A, Loquercio G, Muto P, Apice G et al: Platelet gel in cutaneous radiation dermatitis. Support Care Cancer 2013, 21(1):287-293.

